COURT OF QUEBEC
Criminal and Penal Division
CANADA
PROVINCE OF QUEBEC
DISTRICT OF
MONTRÉAL
CITY OF
MONTRÉAL
No:
500-01-006624-073
DATE:
September 12, 2011
_____________________________________________________________________________
BEFORE THE HONOURABLE JUSTICE LOUIS A. LEGAULT, J. C.Q.
_____________________________________________________________________________
THE QUEEN
Prosecutor
v.
JAMES STEVEN WILCOX
Accused
_____________________________________________________________________________
JUDGMENT
_____________________________________________________________________________
[1] The accused, Mr James Stephen Wilcox, is charged with aggravated sexual assault (section 273 (1) ((2) b) of the Canadian Criminal Code) and aggravated assault (section 268 of the Criminal code) endangering the life of complainant G. W. between July 1st and August 31 2005.
THEORY OF PROSECUTION AND DEFENCE
THEORY OF DEFENCE
NO LIFE ENDANGERMENT TRHOUGH HIV IN VIEW OF SCIENTIFIC ADVANCES
[2] Defence invokes that the sexual encounters between complainant and accused in the current stream of the medical and scientific advances did not endanger the life of the accused.
IMPLICIT CONSENT ALLEGED AT THE SAUNA FOR GAYS
[3] Defence invokes an implicit consent of complainant to a possible HIV infection. Defence invokes it is a well-known accepted reality and that he presumed that people engaged in sexual unprotected activities in sauna for gays who do not put questions on the sexual health or HIV status of their partner, are willing or indifferent to becoming namely HIV infected. He presumed that complainant as a silent partner in a sauna for gays was contextually and implicitly assuming the risks of HIV infection.
DISCLOSURE ALLEGED AS BEING AT THE INITIATIVE OF THE ACCUSED. DISCUSSIONS WITH COMPLAINANT AT THE TIME.
[4] The accused alleges disclosure at his initiative of his HIV status to complainant immediately after their first anal sexual unprotected intercourse at the accused’s residence in July 2005.
[5] The accused alleged that complainant was understanding, did not care whether the accused was HIV infected, was ready to marry him.
[6] Complainant would have stated that he did not know of his HIV status as his yearly tests were passed in 2004 as he would have unprotected sex since the last tests and is alleged to have admitted to having had unprotected sexual intercourses before, that they agreed finally to keep on having sex, dating and being careful.
[7] The accused spoke of his experience of becoming and being told he was HIV positive. Complainant was also invited by the accused to be tested within 3 months and that they would be careful in their sexual intercourses in the future.
[8] Complainant would have made reference to his being home sick and as to his difficulties in his relationship with father. Complainant and the accused would have acknowledged their increased pleasure at having unprotected sex.
[9] The accused thought that complainant was rather safe as the unprotected anal intercourse was not risky as he had ejaculated outside complainant’s anus and reminded complainant to go for the HIV testing within three months which was done in September 2005 and proved to be negative.
[10] Complainant was referred to as dishonest in court although he conceded he was honest in an E-mail of October 2011. Complainant was referred to as naïve and vulnerable through his unprotected sexual behaviour.
CONTINUATION AFTER DISCLOSURE OF BOTH PROTECTED AND UNPROTECTED
[11] Defence alleges the pursuit of both protected and unprotected anal sexual intercourse in a regular fashion between both and their ongoing romantic affair witnessed by the accused friends until some time in October 2005 as their boyfriend’s relationship ended. The most significant risky joint penetration of a dildo and penis anal intercourse would have happened somewhere between August and end of October 2005.
ACKNOWLEDGEMENT OF COMPLAINANT REGARDING SEXUAL BEHAVIOR AND DATING
[12] The accused refers to the acknowledgement of complainant that he did continue to have sexual intercourses with him and wanted to keep dating and was indeed dating as he had a number of meals with the very good friends of the accused and was presented as the accused boyfriends and as both manifested physical tender proximity as confirmed by the testimony of the accused friends. Defence also pleads that the simple fact of complainant entering unprotected sex without any questions to the accused meant he was acting risky and could be believed to have been infected otherwise, at other times or after disclosure and that it is possible complainant in July was already HIV infected.
[13] Defence also alleges that complainant in a suspect way and out of the blues, when testifying, mentioned that he did not know if the friends that he met from July 2005 and are now living elsewhere were HIV infected.
RENTAL OF THE ACCUSED RESIDENCE AS A FAVOR TO COMPLAINANT
[14] The accused confronted with complainant living rather poorly in an apartment and with the sudden inability of a good friend of his to take over his condominium for winter 2005-2006, offered complainant to rent his residence for that period at a cheaper rate than the one granted a friend in the preceding winters. Leaving his condominium unoccupied was not wise.
TIME OF JOINT DILDO PENIS ANAL INTERCOURSE THAT WAS THE MOST RISKY AND IGNORANCE OF THE ACCUSED CONCERNING A TRAUMA THEN SUFFERED
[15] The accused alleges that the joint dildo penis anal intercourse took place somewhere around the end of August or in October 2005. He states his ignorance of the trauma allegedly suffered by complainant until June 2006 after complainant HIV positive testing. The accused cannot be specific on that date, believes it could have happened at the end of August. He is sure that they kept on having sex and dating.
DIFFERENCE IN VERSIONS OF BOTH REGARDING THE DILDO AND POSITION OF INTERCOURSE
[16] The accused states that during this joint dildo penis anal penetration complainant was lying on his belly as he would have been inserted a rather big size dildo and his penis that could not be observed by complainant. The dildo was not a twin dildo as alleged by complainant serving for a double penetration by lovers and complainant’s description was related to as totally unknown to him. The accused said that he gave that dildo to complainant before his departure in November 2005 and denies that complainant offered him in exchange a smaller dildo.
ALLEGATIONS OF UNTRUSTWORTHINESS OF COMPLAINANT AND OF INSUFFICIENT CIRCUMSTANTIAL EVIDENCE
[17] Defence pleads that complainant’s testimony is frail, questionable and untrustworthy. Complainant’s confusion, contradictions, contradicted eviodence by independent witnesses as to dating and uncertainties in events after July 2005 is invoked to question the trustworthiness of complainant’s testimony. Defence alleges also complainant’s multiple contradictions, vague statements and lack of trustworthiness weakens his credibility and that it should adduce reasonable doubt in favour of the accused. His alleged consent in the sauna for gays is invoked, the fact that he would have been in the past as well at all times relevant in that relationship engaging in unprotected sex, the most significant risky HIV sexual behaviour happening after disclosure, his ongoing dating and alleged sexual intercourse after disclosure and the fact that the HIV infection could have come from someone else and several other facts are invoked to allege the accused total untrustworthiness.
CONFUSION OR CONTRADICTED EVIDENCE OF COMPLAINANT REGARDING THE JULY SAUNA GATHERING, THE DATES OF ONGOING MEETINGS AND GATHERINGS AND COMPLAINANT’S BEHAVIOR AND LOVE INTERCOURSE WITH THE ACCUSED
[18] Reference is made to complainant’s weak memory or contradictions as to the sauna policies regarding condoms, as to dates of complainant and the accused gathering. Complainant’s confusion and uncertainties regarding events after July 2005 are invoked to question the whole trustworthiness of complainant’s testimony.
[19] The accused is supported by the statements of account of both telephone and credit card bills and E-mails to which he refers and makes sense of to give an idea of the evolution of their relationship. The accused in a rather precise fashion alleges he recalls ongoing activities, meals, the nature of their dealings, meteo records that were instrumental to their dealings, the extent of exchanges, of phone calls or messages to the best of his recollection.
DEBATE ON DATING WHERE COMPLAINANT ACCEPTED THE ACCUSED OTHER ONGOING LOVE AFFAIR
[20] The accused refers also to a long August 2005 phone call following a meeting where exclusivity was refused to complainant as lover to complainant’s displeasure. The accused describes complainant’s very emotional and adamant reaction to that decision of the accused and his finally yielding to keep on dating after that long phone call. . There would have been an ongoing display of affection, tenderness, love and sexual intercourses.
DATING AND BOYFRIENDS STATUS CONFIRMED
[21] And indeed, the accused and complainant are alleged to have kept dating, there being several gatherings, meals with a number of very good friends of the accused to whom complainant would have been presented openly as his boyfriend. They would have then an openly and privately truly overtly affectionate relationship with namely kissing and touching their buttocks. They exchanged lots of these marks of sensual reciprocity and were in close physical lovers proximity.
ONGOING PROTECTED AND UNPROTECTED SEXUAL INTERCOURSES AFTER JULY 2005
[22] There would save one exception (as immigration was a concern to complainant) at every time they met at the accused residence have engaged in both protected and unprotected sexual and anal intercourses. The first September results of complainant being HIV negative were good news for both.
ONGOING LOVE BY COMPLAINANT AS HE DEVELOPPED A REVENGEFUL ATTITUDE THEREAFTER
[23] Complainant is alleged to have remained very much in love with the accused and hoped for the best and as the weeks passed in October and as it came to an end, it was evident that their relationship would not continue.
OCTOBER 2005 ALLEGATION BY THE ACCUSED THAT HE REFERRED TO THEIR ONGOING SEXUAL RELATIONSHIP
[24] The accused had some critics about complainant in the October 2005 E-mail regarding what could be qualified as an incoherent and risky sexual behaviour of complainant, proposing the interpretation that he was then referring in that first paragraph to their ongoing sexual intercourse.
THE ACCUSED EXPRESSION OF HIS BEING SORRY
[25] Complainant’s demand was also served by the repeated written excuses as the accused said how sorry he was for him as for his 2006 lover who was also infected.
COMPLAINANT ENGAGED WITH ANOTHER PERSON AROUND FALL 2006 AND ALLEGATION OF REVENGE THROUGH THOSE PROCEEDINGS
[26] The accused is aware that around fall 2005, the accused was getting more engaged with another friend that has been his companion since then. But he alleges that complainant remained very attached to him and revengeful as the accused truly was in love with a Mr D. at the beginning of 2006.
[27] Defence alleges complainant’s multiple contradictions and lack of trustworthiness also weakens his credibility and that it should adduce reasonable doubt in favour of the accused all the way through.
PERIOD OF INTIMATE SEXUAL ENCOUNTER BETWEEN THE ACCUSED AND COMPLAINANT
[28] Both complainant and the accused in their very first statement to the police had stated that their relationship ended in August 2005. In Court, the accused alleges their sexual encounters ended in October 2005 contrary to complainant who alleges it did end in August 2005. Confronted with the telephone records of July 2005, complainant recognised that they met until October 2005 [1].
[29] Complainant is also challenged on his indebtedness to the accused regarding the rental of the accused ‘s residence during winter 2005-2006.
[30] The accused opposes to his 2007 statement to the police the fact that after review, his telephone and credit card accounts and E-mails are a clear reminder of clearly of a longer period of intimacy and relationship between both. These accounts allegedly give credit to his detailed version of facts and to his allegation of revenge on the part of complainant regarding the accused refusal to engage more in a relationship with complainant.
ALLEGATION OF JEALOUSY AND REVENGE
[31] The accused alleges that complainant was simply jealous, revengeful and wanted so much sexual exclusivity with the accused although they kept on dating and was presented as his boyfriend that his account of facts is not trustworthy. Confronted and refusing dating in those circumstances, complainant would have accepted to dating which he would have done in reality accompanied with sexual intercourses.
[32] The first September results of complainant being HIV negative and brought some welcome temporary relief.
[33] Complainant is alleged to have remained very much in love with the accused and hoped for the best and when October came to an end, it was evident that their relationship had come to an end and would not continue. Complainant was in love with that person he worked for in the vicinity of [Company A] in the Old Montreal.
[34] The accused kept on dating Mr M. F., another gentleman, during the summer of 2005 and felt in love at the beginning of 2006 with a Mr D.. The complaint would have been laid according to the accused as a means of revenge as complainant invented and distorted the facts and falsely charged the accused.
ABSENCE OF SCIENTIFIC TESTS CONTRIBUTING TO ESTABLISH THE ACCUSED’S RESPONSIBILITY IS ALLEGED FATAL TO PROSECUTION
[35] Defence alleges the absence of any scientific evidence (philogenetic or genotypic tests) linking the genetics of the HIV condition of both the accused and complainant. Defence points out to the fact that as the first test was done in September 2005, the second test should have been administered around February, not in May and June 2006. The delays in testing according to the accused also contribute to question his guilt or at least give credit to the alleged traumatic intercourse that happened later in the summer or at the beginning of fall 2005.
THEORY OF PROSECUTION
COMPLAINANT’S ALLEGATION OF ONLY ONE UNPROTECTED AND ALLEGEDLY VERY SIGNIFICANTLY RISKY TO THE POINT OF ENDANGERING HIS LIFE AT THE ACCUSED RESIDENCE AFTER A ROUND OF PROTECTED SEXUAL INTERCOURSES AT THE SAUNA OASIS
[36] Complainant states that after oral sex and caresses at their first gathering at the Sauna Oasis, he started by having anal protected sex on plaintiff and that after, the accused did the same on him and that this ended their round of sexual intercourse followed by a shower and the accused taking complainant near his home and exchanging information regarding their phone numbers.
[37] Prosecution alleges that the HIV infection of complainant happened in their first and only unprotected joint dildo and penis anal penetration of complainant at the residence of the accused. That penetration caused trauma and complainant was infected through the emission of pre-ejaculatory liquids of the accused that preceded his ejaculation outside complainant’s anus.
[38] That conduct is alleged to have endangered complainant’s life. The expert is clear that even with pre-ejaculatory liquids, HIV will rapidly infect an anal mucus damaged and bleeding although with a sane one, the risk would be less significant but still real.
ABSENCE OF DISCLOSURE ALLEGEDLY A FRAUD VITIATING COMPLAINANT CONSENT
[39] Prosecution pleads that their first risky unprotected sexual anal intercourse at the accused residence became an assault as consent was vitiated by the non-disclosure by the accused of his HIV status. Prosecution denies tacit or contextual consent of complainant at the sauna, the absence of any other sexual intercourse after the first gathering at the accused residence and the admission of the accused that can be inferred in an E-mail to complainant regarding complainant’s infection. Complainant if informed of the HIV status of the accused would clearly have refused to have sexual intercourse with him.
[40] The accused confronted by complainant said he thought complainant was HIV at the sauna Oasis.
[41] Complainant states that after their sole unprotected joint dildo penis sexual intercourse as he became aware that the accused was also inserting his penis, his anus bled all day and he came back at the accused domicile and accused upon his questioning disclosed his HIV status. Very excited, the accused came to orgasm rapidly after outside complainant’s anus.
[42] As complainant was furious at himself and at the accused, the accused both tried to reassure him, tell him he had to protect himself for 3 months and as he did not ejaculate in his anus, the results should be favourable. He spoke of all the distress he went through when so advised in 2003 of his condition.
[43] Complainant said if he had known the HIV positive status of the accused, he would certainly not have had any unprotected sexual intercourse with the accused but would have considered taking measures to be with him in consulting if he had been frank. Complainant would not have risked the HIV infection.
[44] He said how he truly hated the accused for being infected and his guilty silence. The accused admitted to complainant that he was not keen on using saves. The accused would have stated that he was fed up being treated « as shit » as he was HIV infected.
COMPLAINANT’S AND UNPROTECTED SEXUAL INTERCOURSE
[45] Complainant is clear that he did not in the past have sex without the protection of saves except for oral sex. He says he was HIV negative as he goes for testing yearly, as he never risked unprotected sex even when he acted once in a XXX film. Complainant never expected the accused to take advantage of him and remain silent making him risk that infection he is now caught up with.
[46] Complainant states that since September 24 2005, he has a love in his life. It has been going on for four years. Until 2006, they had protected sexual intercourses and since then they only have oral sex and his companion has no HIV infection.
[47] Complainant states that he stayed in touch with the accused to keep track of him and that he had no more sex and did not come to an agreement with the accused regarding dating him because the accused refused him the exclusivity of intimacy.
HIV INFECTION OF COMPLAINANT CAUSED BY THE ACCUSED
[48] It is alleged that the circumstantial evidence disclosed leaves no doubt as to the HIV infection of complainant by the accused. That would be so in the opinion of Prosecution as it directs its pleadings on the alleged frailties and total unlikelihood of the accused pretences whatever were the loopholes and apparent frailties of complainant testimonies and on the solid evidence linking the accused to his HIV condition.
[49] Furthermore, the Court is invited to give weight to the fact that within the next two months, the symptoms of which complainant suffered are compatible with the first symptoms of an HIV infection that should be kept in mind as it follows within less than three months an alleged traumatic anal intercourse very likely to cause rapidly an HIV infection.
PERIOD DURING WHICH BOTH THE ACCUSED AND COMPLAINANT WERE INTIMATELY SEXUALLY INVOLVED
[50] Complainant is blunt and allegedly constant that he did not have any other sexual encounter after July 2005 except with his companion since September 2005 until 2006.
[51] Prosecution refers to the fact that both complainant and the accused thereafter in their statements to the police believed that their sexual endeavour took place in August 2005. The accused through his records corrected that impression by establishing that the very specific events mentioned happened a few weeks before in the month of July 2005. Moreover, the accused is also the one who amongst his remarks to complainant spoke of that first 3 months waiting period for testing and of the necessity of protecting him in his sexual encounters.
ADMISSION BY THE ACCUSED IN HIS OCTOBER 2006 E-MAIL
[52] Prosecution alleges that there was a clear admission by the accused regarding his responsibility for the contamination of complainant in an E-mail dated October 14, 2006. The accused would then have stated what is an admission that should set aside according to the Prosecutor any defence on the counts as pursued[2].
[53] The accused was clear that he did not disclose his condition as he was fed up being treated like « shit » as he would have stated to complainant.
ACCUSED CONTEMPT OF COMPLAINANT
[54] The accused E-mail continues and it has to be examined as it attempts to defeat the impression left on complainant that would give credit to the accused’s contempt, belittling and absence of consideration for complainant[3]. Certainly that no one is perfect or meets necessarily the fantasies of personal expectation regarding their partners.
MANIPULATION OF COMPLAINANT IN VIEW OF AVOIDING CRIMINAL PURSUITS
[55] That negative opinion of complainant by the accused could characterise the actions of the accused as being manipulative, not sincere, headed to help avoid or reduce any possibility of criminal pursuits. In feeling bad about that undisclosed HIV risky sexual encounter, the accused took steps to be more inclusive and be very nice to complainant.
[56] No doubt that the accused could find complainant to be otherwise a decent man although not fluid in the English language and although it can be questioned whether truly the accused considered complainant as a boyfriend. There is no doubt that the accused had no plans for the future with complainant and that must have left no doubt in his refusal of sexual exclusivity with complainant and his ongoing affair with Mr Fo..
[57] The serious risk of HIV infection of complainant got the accused to be legitimately nicer with complainant in taking initiatives of dating and shows of love and renting of his residence to earn the indulgence of complainant.
EXCLUSIVITY OF COMPLAINANT’S RELATIONSHIP AND DATING
[58] Complainant denied he would never have accepted and did never accept to date the accused as he was insisting on dating a Mr Fo.. That was unacceptable to complainant.
[59] Complainant will reaffirm throughout his testimony that after July 2005, even after meals or walks, he never engaged in more sexual intercourses. A friend of the accused with whom complainant and that accused had dinner, was surprised that if they were boyfriends, complainant did not accept joining to go dancing after.
SIGNIFICANT RISK OF THE JOINT DILDO PENIS PENETRATION
[60] Prosecution alleges that an anal unprotected intercourse when there is an exposure to pre-ejaculatory liquids is significantly risky. The expertise speaks as to a much more significant risk of infection when there is a traumatic anal sexual intercourse and exposure even to pre-ejaculatory liquids. It is strongly alleged that it happened in July in their sole intercourse at the accused residence.
ANALYSIS OF THE EVIDENCE
[61] The Supreme Court of Canada and several decisions of the Appeal Court of Canada have reminded that the accused benefits from a presumption of innocence until judgment, that the burden is on the Crown to establish the guilt of the accused, that if the accused’s version is trustworthy and raises a valid means of defence or otherwise if the version of the accused raises a reasonable doubt in the context of the whole evidence, he should be forthwith acquitted.
[62] A negative answer to these two tests would leave on the Crown the burden of establishing the guilt of the accused beyond a reasonable doubt[4].
[63] At every step of analysis of the evidence, it would be an error to assess it in a vacuum as Justice Beauregard of the Appeal Court did so well put it[5].
[64] The Supreme Court has reminded that all of those principles of assessment of evidence, of trustworthiness of witnesses or of presumption of innocence are not a matter of form but substance. In any case, the workings of interpretation of the presumption of innocence command a careful examination of all of the evidence to ascertain if guilt is established beyond a reasonable doubt or if a reasonable doubt remains.
[65] Judge Healy comments on how to approach the Supreme Court of Canada analysis of evidence is enlightening. « The credibility of witnesses is a central component in the assessment of the evidence on the whole of the case. This is not only so where there is a conflict between evidence for the prosecution and evidence for the defence… Moreover, questions of credibility are not restricted to gaps or conflicts in testimony. In every case the ultimate question remains whether on the whole of the evidence guilt has been proved beyond reasonable doubt[6].
[66] « More recently the Supreme Court has emphasised that the guidance in W.(D.) is not a dogma in which form should be prized over substance. It is a reminder of the relation between questions of credibility and the practical application of principles that inhere in the presumption of innocence. An assessment of the evidence on the whole of the case necessarily means that all of the evidence of every witness must be fully considered. To this end the Court has said that there is no single way in which to proceed, provided that it is made clear that credibility is an important element in weighing the persuasive strength of the evidence as a whole. »[7]
[67] Whatever conclusions judges come through, they have a duty to justify that they have weighed the whole of the evidence, as it is a rule of justice that any reasonable doubt benefits an accused. Judges have to carefully, courageously, impartially and insightfully assess the whole evidence with an open mind. Judging is quite a terrible and burdensome privilege as a judge should not yield to any ill-temptations of popularity that do not reconcile with those highest timeless responsibilities meeting the core values of that justice to be rendered and appearing to having been so done.
[68] In the stay of Lifchus, the majority stated that a Court is not to speculate on where the truth lies and that a doubt that is reasonable cannot be a frivolous doubt or born through his imagination, it cannot rest on sympathy or on prejudice. Good sense and reason must guide the Court and the verdict must flow logically of the evidence or of the absence of evidence[8].
[69] To terminate these considerations on how to apply the law fairly and equitably, the Court will quote and translate from its French version the opinion of late Justice Michel Proulx of the Quebec Court of Appeal, one of our most learned jurists who was totally dedicated to explaining the law. On contradictory versions, late Justice Proulx expressed the opinion that « it was worth repeating that a trial judge… did not have to decide to reach a verdict on which of the versions wins over the truth… but if the evidence all considered satisfies the Court beyond a reasonable doubt of the guilt of the accused, consequently the accused does not have to meet a burden to show that the victim does not state the truth…The Prosecutor has the burden to establish that the truth proposed is shown beyond a reasonable doubt. The burden of that truth has always to be met by the Prosecutor. To require the accused persons to show the lie of complainants would atrophy the presumption of innocence. A reasonable doubt surges if the Prosecutor fails in its attempts to convince the Court of its truth. »[9]
ADMISSIBILITY OF A TESTIMONY OF A DEFENCE WITNESS TO SERVE AS EXPERT EVIDENCE ON THE CREDIBILITY OF A TACIT CONTEXTUAL CONSENT TO SEXUAL INTERCOURSE BY GAYS IN A SAUNA.
[70] Prosecution objected to the testimony of Mr Rousseau who was presented as an expert in the field of gay behaviour and interpretation of that behaviour in saunas reserved for gays. That testimony was received under reserve.
[71] The evidence of an expert is only admissible if it is relevant, material and necessary as stated in Mohan[10].
[72] The expert is manifestly knowledgeable about the culture of gay people, his theory a representation or personal understanding here and now of part of the reality of gay people who attend sauna for gays locally.
[73] The expertise of Mr Rousseau relates to a silent understanding in gay saunas that those who have unprotected sex with strangers without disclosing their respective HIV status are namely people who are or HIV infected or are ready to risk so being infected and are indifferent to that possibility. He offered an expertise regarding the assessment of complainant’s behaviour and a so-called tacit consent to be inferred from the attendance in these saunas reserved for gays.
[74] That gentleman offers no scientific expertise but just an opinion that has nothing scientific, nothing but a psycho-sociological understanding and generalisation of the behaviour of some of those who engage in risky sexual practises in gay saunas. His opinion weighs and interprets the conduct of people attending gay saunas and the probative value of the testimony of the accused and of complainant. He testifies about his views about a silent consent of partners and on the contextual understanding of sexual mates entering saunas for gays when there is no disclosure of their HIV status.
[75] In this matter, as it is a matter of opinion, it clearly is the responsibility of the trier of fact to make inferences or draw conclusions and to adjudge on the credibility of the witnesses and to draw inferences and conclusions from the non-expert evidence heard[11]. The possibility or likelihood of it being an implicit consent does not suffice to render that testimony an expert testimony as it has nothing scientific and as it is not necessary.
[76] On the grounds of necessity and absence of scientific expertise of the witness, this so-called expertise fails and is not admitted in evidence.
APPLICABLE LAW
RULINGS REGARDING AGGRAVATED ASSAULTS ENDANGERING THE LIFE OF A PERSON
[77] Section 265 of the Canadian Criminal Code defines assault as follows. « (1) A person commits an assault when (a) without the consent of another person, he applies force intentionally to that other person, directly or indirectly; (3) For the purposes of this section, no consent is obtained where the complainant submits or does not resist by reason of (c) fraud ».
[78] In R. v. Mabior, the accused was charged with having both protected and unprotected sexual encounters with several complainants. In addressing whether endangerment of life had been proved in relation to aggravated sexual assault, McKelvey J. adopted the language of Cory J. in R. v. Cuerrier and held that “the potentially lethal consequences of unprotected sexual contact leave room for no other conclusion than that endangerment of life has been substantiated.” He also referred to the language of the Ontario Court of Appeal in R. v. Thornton (1991), 82 C.C.C. (3d) 530 at 531: « When the gravity of the potential harm is great, in this case “catastrophic”, the public is endangered even where the risk of harm actually occurring is slight, indeed even if it is minimal ».
[79] The Prosecution needs to prove that the life of complainant was endangered by the acts of the accused[12].
[80] There has to be a significant risk of serious bodily injury that actualises consequently an absolute duty to disclose. The duty to disclose increases as the risks of serious bodily harm becomes significant. That risk of harm cannot be trivial[13]. The greater the risk of deprivation, the higher the duty to disclose[14]. The failure to disclose the HIV infection fulfills the requirements attached to fraud, which is dishonesty and deprivation or risk thereof[15]. That dishonesty is to be assessed objectively[16].
[81] Prosecution has to establish that there was an intentional application of force without the consent of complainant[17] and an objective foresight of the risk of bodily harm[18]. The Consent[19] is valid if it is informed, clear and unequivocal[20] and flows from the knowledge of the status of a partner upon who lies the duty to disclose his HIV status[21]. The absence of consent is assessed by reference to the complainant’s subjective internal state of mind toward the touching at the time it occurred.[22] The failure by an HIV infected person to disclose his HIV status vitiates the consent to engage freely in a sexual intercourse.
[82] Furthermore, there shall be no reasonable doubt that complainant would not have engaged into a significant risky sexual intercourse if there had been disclosure of the HIV positive status of the accused[23].
[83] In the case of Williams[24], the Supreme Court of Canada pronounced a verdict of guilt on a charge of attempt [25] to commit an aggravated assault as it could be inferred that most likely, the victim was infected at the time of the sexual intercourse by that accused who ignored his VIH positive status.
CONTENT OF EXPERT EVIDENCE REGARDING THE HIV INFECTION
[84] The Court benefited from the expertise of a learned specialist, Dr Richard Morrissette. Here is the summary of what the expert stated[26].
[85] Untreated, the HIV infection is lethal.
[86] Without medication, HIV infected people can survive between 10 and 13 years. It is a chronic disease. It cannot generally be cured. The infection can be controlled.
[87] The HIV virus is disseminated through the blood. It can infect a human body namely through the sperm, the post and pre-ejaculatory liquids, through vaginal or anal contacts, through the blood.
[88] HIV can be disseminated through unprotected vaginal or anal sex. A healthy vagina may be less conductive to an HV infection than a healthy anus. However when damaged, confronted with the HIV infection, these tissues are highly vulnerable to becoming rapidly infected.
[89] If infected sperm, liquids or blood infect a sane person, even if it is less likely with pre ejaculatory liquids, the risk of a rapid infection becomes major, most significant and important if at the time of an anal intercourse for example, the mucuous of the anus has been damaged and is exposed to pre-ejaculatory liquids. That risk with a sane anus for example remains real, significant although lighter. One sexual unprotected intercourse will suffice in the case of an anal intercourse where the anus is damaged and where a partner is about to ejaculate, as it is very likely that pre-ejaculatory liquids will flow in the anus.
[90] Oral sexual intercourse is hardly conductive to HIV infection unless there are health problems in the mouth.
[91] The HIV virus is diverse and at times not easily countered. As the HIV infection is an evolving complex virus, new treatments and medication is invented to counter HIV infections and Aids.
[92] The HIV virus can remain alive on an object between 48 and 72 hours. But left in the sun, that HIV virus will last at most 3 hours.
[93] Fatigue, mononucleosis, diarrhea, swollen ganglions are amongst the first symptoms that will appear.
[94] At this period of time, most people may get cured through the administration of a massive dose of medication within 3 days of the risky sexual encounter.
[95] Properly medicated, an HIV infected person’s life span expectation expands to approximately 80 years old. As they are aging, their anti-body is likely to become undetectable. Then they are likely to die of opportunist infections that will strike them, as they are not any more immune as medication for the HIV or AIDS infected persons will not foster and maintain their immunity. The expert said that generally, HIV infected persons do not die of the direct consequences of the HIV infection of AIDS.
[96] Tri-therapy medication helps generally counter the evolution of HIV, as there are several types of medication to control diverse virus. Medication exists today that can help block the entry or the exit of the virus in the cells and reduce it below levels considered at risk.
[97] If well treated and under very close supervision, protective cells can be increased in numbers favouring the defence of the organism as it can induce a negative viral charge after a number of years. USA health institutions have come to conclude that there may circumstances where the viral charge appearing negative, there can be safe sex without contraceptives. If properly treated, then HIV infected people viruses proliferation can be blocked, so that HIV infected persons would not endanger the life of others in sharing unprotected sexual intercourses.
[98] Multi-disciplinary teams nowadays follow HIV infected persons and explain the disease and its consequences, their responsibilities. They are recommended to advise their partners of their illness. There is an absolute necessity for HIV infected persons regarding unprotected sexual intercourse to disclose their health condition as medically stated by the expert. They are being told that condoms well used are generally efficient.
[99] There are .4 of 1 % or less risks of transmission of HIV by fellatio. Risks are truly increased and even real if a partner has a poor dental health.
[100] Properly protected intercourses protected adequately with the use of a latex prophylactic is considered to reduce the risks of HIV infections to below any significant risk.
[101] It took 6 months in 2006 for tests to show the HIV infection. Nowadays, it takes 3 months to get the HIV results.
DETAILED FACTUAL NARRATION
KNOWLEDGE BY ACCUSED OF HIS HIV STATUS SINCE 2003
[102] The accused knew he was HIV infected as of 2003 whereas complainant got the HIV positive testing news in May and June 2006 after a September 2005 clearly interim negative HIV testing passed after a number of compatible HIV symptoms hit complainant.
FIRST SEXUAL ENCOUNTER AT THE SAUNA FOR GAYS
[103] At the beginning of July 2005, on their first meeting in a sauna reserved for gays, complainant and the accused had sexual intercourse. Complainant and the accused first testified it happened in August 2005. That was the period alleged for their lovers’ relationship in the statement to the police in the following years.
SOMEWHERE IN JULY, AT THE ACCUSED RESIDENCE, UNPROTECTED SEXUAL ENCOUNTER
[104] The accused and complainant engaged in unprotected sexual intercourse at a gathering at the accused residence within a short time after their meeting at the sauna for gays. It was around the July 21, or days before as complainant who is not to keen on dates felt.
DISCLOSURE BY ACCUSED OF HIS HIV POSITIVE STATUS
[105] Disclosure was made by the accused after that intercourse. Versions differ as to the content of the discussions and as to the emotions displayed. However, The accused stated he attempted to reassure complainant as there had been no ejaculation within his anus and as it should be confirmed by proper testing within three months.
IF THERE WERE ONGOING SEXUAL INTERCOURSES BETWEEN THE TWO, THEN COMPLAINANT HAD TO BE FULLY INFORMED.
[106] If there were any sexual intercourses after the one at the residence of the accused, then any such sexual intercourse took place with complainant fully informed of the accused HIV positive status. The accused and complainant kept gathering, did hike together, shared meals, had diners with the accused friends on a few occasions as he was presented as the accused boy friend.
[107] The accused rented his residence to the accused during the winter 2005-2006.
REGULAR CONTACTS AND GATHERINGS OF BOTH
[108] Complainant and the accused stayed regularly in touch by phone and E-mail and met from time to time and complainant was made to meet the accused friends in August and October 2005. Complainant was then presented as the accused boyfriend.. They had meals together and even met at the accused residence
[109] Then, there were these communications as complainant accepted to become the lessee of the accused who went down south and as the positive results of the HIV testing of complainant got them to interact as well as some allegations of unpaid rental obligations of complainant.
CURRENT BEHAVIOR
[110] They met as the accused was committed to another gentleman with whom he was involved sexually and kept on doing so as he did not wish to abandon that relationship. They both attended saunas for gays before they met. Complainant became involved with a friend during the course of fall 2005.
FIRST TESTING IN SEPTEMBER 2005, SECOND IN MAY 2006 AND A THIRD IN JUNE 2006
[111] Complainant did undergo a first HIV testing in September 2005 as he had been sick and was informed that he was HIV negative. He was told that he should undergo further testing within the 6 months of that risky sexual encounter. It would then be expected that the next testing would take place around February 2006. Tests were conducted in May and June 2006.
[112] Complainant went through periods of fatigue in the winter of 2006 from January on. The results of his tests dated May 17 and June 21, 2005 revealed complainant to be diagnosed as HIV positive. The accused was rapidly informed of those results.
RECORDED INTERVIEW AND E-MAIL OF OCTOBER 2006 OF THE ACCUSED.
[113] Complainant attempted to obtain a secretly recorded confession of the accused in which he stated as a preamble to a question that they had kept on having sex and dating after their sauna intercourse. Complainant submits an interpretation of what he meant and discussions on their wanting to date and their meeting and on what meant their ongoing sex.
[114] Later on, at complainant’s invitation by E-mail dated October 14, 2006, the accused expressed regrets and admitted by E-mail his difficulty in voicing and disclosing his HIV positive status[27]. He was morally unable to do so. He expressed repeatedly how sorry he was for complainant being infected and his thinking that situation over and over and his being surprised at complainant’s not thinking right and being or acting vulnerable.
[115] There are further allegations by the accused that in his E-mail of October 2006, he was referring to an ongoing sex life with complainant, which is denied.
[116] The accused described complainant as decent and honest in his E-mail. That was one year and 3 months after their July encounters at the Sauna and at the accused residence.
DILDO PENIS JOINT PENETRATION ADMITTED, BUT NOT THE KNOWLEDGE OF ANY TRAUMA SUFFERED NEITHER THE JULY DATE
[117] Defence acknowledges that there was indeed at one time a dildo penis penetration. He says he remained ignorant of the trauma suffered by complainant and sets the time frame rather somewhere in August or October 2005. Complainant alleged hat it is that intercourse at the accused residence in July 2005 that worried him and got him to confront the accused as he has suffered a trauma that he denounced to the accused after disclosure.
NUMEROUS E-MAILS EXCHANGED
[118] There were indeed a number of E-mails exchanged that were produced and sggest inferences of the relationship of complainant and the accused and have relevancy to point to the reality of ongoing exchanges.
DISPUTED FACTS
IMPLICIT OR CONTEXTUAL CONSENT OF COMPLAINANT
[119] Was there an implicit consent on the part of complainant expressed as the accused and complainant first met in a sauna for gays? Did complainant flag the fact he was a bug chaser (someone not HIV willing to be HIV infected) or that he was HIV positive? Is there evidence of complainant subjectively accepting that risk?
WAS THERE A SECOND ROUND OF UNPROTECTED ANAL INTERCOURSE AT THE SAUNA FOR GAYS? WAS THE ACCUSED HAPPENED TAKEN BY SURPRISE?
[120] Was there possibly an unprotected sexual anal intercourse in a second round of sexual encounters at the sauna as the accused alleges? Would complainant have taken by surprise the accused by his rapidity of execution in entering in his anus the penis of the accused?
FAILURE TO DISCLOSE, TIME OF DISCLOSURE, INITIATIVE OF DISCLOSURE AND CIRCUMSTANCES OF DISCLOSURE
[121] The accused acknowledges that he did not disclose his HIV positive status to complainant until after the second sexual intercourse at the accused residence. He alleges the continued tacit contextual consent that should be inferred from their first place of gathering and complainant’s behaviour.
[122] When did the unprotected intercourse at the residence of the accused take place? In the afternoon of their meeting or on the following morning as complainant alleges that it is then that there was sexual intercourse? Was it a simple unprotected anal sexual intercourse or was it a traumatic joint dildo penis anal penetration of complainant by the accused?
[123] Who took the initiative of disclosure or asking disclosure? When did it happen? Was there a traumatic intercourse?
[124] Whenever there was that traumatic intercourse, was the accused advised of the trauma suffered by complainant?
INITIATIVE OF DISCLOSURE, CIRCUMSTANCES OF DISCLOSURE AND SURROUNDING DISCUSSIONS
[125] The accused and complainant both claim they are the ones who took the initiative regarding disclosing or asking for transparency as to the sexual health of the accused.
[126] There are neat differences in the account of the time and circumstances of disclosure. The accused referring to discussions he had with complainant after disclosure relates in a totally different fashion the ongoing discussions Was complainant so neutral or almost as to that infection? Was he already so attached to the accused that he was ready to marry him? Was complainant so unsure about his HIV status that there was no shock regarding having unprotected sex with the accused? Is it likely or possible that complainant would have been reacting rather as being home sick or relating forthwith his difficult relationship to his father. Is it likely or possible that they would have exchanged on the pleasures of sex without condom.
[127] Or was complainant upset and flabbergasted upon disclosure? Was he coming back allegedly at the accused residence suffering from a trauma as his anus kept bleeding after a July 2005 morning joint dildo penis anal penetration? He stated the trauma suffered. Both speak to the effect that the accused simply tried to reassure him, to calm him down as there was no ejaculation in complainant’s anus and as testing within the following 3 months could affirm an HIV negative status.
NATURE OF THE RELATIONSHIP BETWEEN COMPLAINANT AND THE ACCUSED AFTER THAT FIRST RESIDENCE UNPROTECTED ANAL SEXUAL INTERCOURSE
[128] Does the material evidence tendered by the accused referring to a number of telephone bills, credit card accounts E-mails and close friend testimonies and E-mail tend to raise a reasonable doubt on complainant having both protected and unprotected sex and kept on dating from august to October? Does the allegation of complainant of his entering a September 2005 love relationship with someone still his companion and still HIV negative together with the continued dating of a lover by the accused contribute to answering the question of guilt. Does all of the tenderness as boyfriends manifested between complainant and accused until October justify a finding of reasonable doubt in favour of the accused?
[129] Does the apparent weakness or confusion or contradicted untrustworthy evidence in the testimony of complainant leave a reasonable doubt as to the guilt of the accused, such evidence relating to dating, to meetings of both and meals even with friends of the accused, those abundant phone calls, many E-mails, close tender physical proximity and boyfriends apparent meetings.
[130] Does the rental situation of the accused residence for the winter 2005-2006 as negotiated, a possible hidden motivation to avoid any complaint has any bearing on the facts of the case? Does the possible indebtedness question the accused trustworthiness or does complainant’s attitude question his trusworthiness?
QUESTION OF COMPLAINANT ONGOING SEXUAL INTERCOURSES WITH THE ACCUSED OR OTHER SEXUAL PARTNERS BEFORE OR AFTER THE JULY INCIDENT IN SIGNIFICANT RISKY SEXUAL ENCOUNTERS
[131] Is it possible that notwithstanding complainant’s denial, he could have engaged in significant risky sexual intercourses at any relevant time other than July 2005 with the accused or with anyone else at all relevant times? Depending on the answer, if affirmative, does it raise a reasonable doubt taking into account complainant’s denial notwithstanding his peculiar declarations?
JEALOUSY AND REVENGE ON THE PART OF COMPLAINANT INVOKED TO EXPLAIN THE MOTIVATION OF COMPLAINANT TO LIE AND DISTORT FACTS FOR THE ACCUSED TO BE FOUND GUILTY OF THE CHARGES AS LAID
[132] Is jealousy or revenge likely or possible to motivate complainant and have him charge the accused when the truth would be not that affirmative and would leave place for a reasonable doubt?
AMENDMENT AND TRUSTWORTHINESS
[133] The attorney for the accused pleaded that as during the accused testimony reference was made to a date of infraction being in July 2011, the Court had in amending the indictment to include the month of July in the period of commission of the infraction of aggravated assault, so confirmed the trustworthiness of the accused. The amendment should be considered as confirming the trustworthiness of the accused versions, so claims the defence.
[134] Defence invokes that there can be no amendment unless a trial judge has such evidence. Defence invokes the fact that it should have been evidence as adduced by the Crown[28]. The amendment could only be used to adduce trustworthiness of an accused.
[135] Indeed, there was an amendment ordered by the court during the course of the accused testimony as the accused appeared to state in a likely way that the sexual encounter or encounters between both that could have infected complainant with HIV and as dealing with exactly the same circumstances of the gatherings at the sauna and at the accused residence before any disclosure could truly likely have taken place in July rather than in August 2005. This is no surprise and was not of a nature to prejudice the accused defence as both were speaking of their sauna and accused home gatherings. It certainly asserts the likely and even sure happening of some of the main events not only in August 2005 but also in July 2005.
[136] Does it discredit per se the version of complainant, that is another question alike all those questions where complainant has a version that differs from the one of the accused on some of the other facts where there are serious grounds to believe that the accused was generally truthful.
[137] That the Supreme Court of Canada has settled debate on March 21, 2011[29], as a verdict of guilt for an offence committed some considerable time before as both parties were then referring clearly to the same events was maintained, thus setting aside any worries of prejudice, any prejudice whatsoever. The evidence upon which a conviction was maintained referred to an infraction that was committed a long time before the one appearing in the indictment. In our case, the difference in time is of at most a few weeks from the month of August mentioned in the indictment.
[138] The Supreme Court majority agreed with the conclusion of Duval Hesler J.A., who dissented in the Court of Appeal, as she expressed the view that [translation] “trial fairness was not compromised. The evidence accepted by the trial judge satisfied her beyond a reasonable doubt that the incident in question did in fact occur regardless of the exact time it took place” (para. 69). In our view, (she states) the defence was based entirely on a question relating to credibility. The respondent was in no way prejudiced.[30]
[139] Therefore if there was no need to so amend manifestly according to that ruling, the amendment authorised did not present any prejudice to the accused whose testimony regarding the infraction was referring to the same events where the infraction is alleged to have taken place. However, the amendment as ordered by the Court, invited to keep the focus on the essential of the case without in any way prejudicing the defence case.
FINDING OF MATERIAL FACTS
IS THE TESTIMONY OF THE ACCUSED TRUSTWORTHIY? DOES HIS VERSION RAISE IN THE CONTEXT OF THE WHOLE EVIDENCE A REASONABLE DOUBT? IF THE ANSWER IS NEGATIVE TO BOTH, DOES THE CROWN ESTABLISH THE ACCUSED GUILT BEYOND A REASONABLE DOUBT?
[140] The Court is unimpressed by the accused testimony relating to an implicit consent of complainant and relating to disclosure. The accused’s testimony is also totally unlikely regarding a major part of the discussions during disclosure such as a demand of marriage, such as the indifference of the accused as to that possible infection.
[141] The accused E-mail admission of October 2006 reads as follows: « I hope that in the future I can accept my HIV status in my daily life so that this is not a dirty secret that I feel like I am hiding. If I do have any other sexual partners, I plan to be totally honest and practice safe sex ».[31] Furthermore, he had clearly admitted to the complainant that he felt «like shit» and was not able to so disclose.
[142] The Court disbelieves the accused pretences that getting sexually involved in a sauna for gays, he did or could take for granted in the circumstances that complainant was HIV positive or indifferent to being HIV infected. Indeed there may be a number of gays ready to so behave and risk that much. That is magic thinking or wishful thinking and does not at all have any air of reality that the accused could think that way seriously.
[143] The facts above from showing that the accused knows that there may be people ready to risk that much, do not at all show in any way whatsoever complainant subjective clear and unequivocal consent to engage sexually with a potentially HIV infected male and risk that much. No evidence supports any such conclusion.
[144] The accused affirmations of his belief that complainant is a «bug chaser» ranks at best as a pure magic thought that has nothing to do with complainant’s reality. It is no more than a simple manoeuvre on the part of the accused to generalize a surprising reality that may be the one of some gays attending saunas in view of his inability to disclose or otherwise hoping for the best.
[145] It is a hope entertained by the accused to release him morally as he also knows that there were at least with unprotected anal sex some risks of HIV infection or even cross-contamination. It was a pretext and nothing more to justify his shortcomings, his moral inability to disclose.
[146] It cannot be said that the accused expectations that a partner should enquire on the HIV status of his partner would not be a responsible and ethical move to be made by partners engaging namely for the first time in sexual activities whether protected or unprotected with a stranger.
[147] That ethical non legal point of view has a clear legalized binding counterpart, a legal and burdening duty binding HIV infected sexual partners to disclose their HIV status to their to-be partner when engaging in significant risky sexual behaviour.
[148] That allegation of a second round of sexual intercourse, this time an anal unprotected intercourse, was meant to serve his alleged defence of implicit or contextual consent that could then be invoked again at his residence based on what would have been that essential implicit consent.
[149] Facts as related by the accused do not in the opinion of the Court permit per se an assumption that complainant consented implicitly to risking an HIV infection.
[150] The accused alleges that complainant took the initiative of a second round of unprotected sexual intercourse at the sauna on their first intimate gathering. Accused then would have had no time to counter that alleged initiative of complainant who after stimulating again his penis into a second erection, would have surprisingly introduced it in his anus. Both would have reached orgasm, as both were very excited. Ejaculation of the accused would have come rapidly after withdrawal of complainant’s anus and masturbation.
[151] These circumstances did not release the accused of his obligation of disclosure of his HIV status. There is no defence whatsoever of implicit or contextual consent of complainant that can be opposed in these circumstances as it would have needed to meet the ultimate burden of there being a clear and unequivocal consent on the part of complainant.
[152] The accused is disbelieved that there was a second round of unprotected sexual intercourse at the sauna. Complainant’s allegations regarding the absence of a second round of unprotected intercourse is believed. In the affirmative, the accused wanted to use that second round as a show of the accused indifference to whatever the HIV status of the accused is. But at the same time, complainant was not any less at a significant risk of the HIV infection. It was meant to show that complainant was indifferent to having unprotected sex and could already be infected before the sauna sexual gathering.
[153] In fact, the accused on that is totally disbelieved.
[154] As the expert situated that unprotected anal intercourse alleged amongst significant risky intercourses even if less than if there had been a damaged anus, the accused would have had a clear obligation to disclose, to make the moves to impeach the accused to do so if he did not want to disclose his HIV positive status.
[155] There was time for disclosure, to withdraw or impeach that unprotected intercourse of going on. The accused is not a powerless victim of complainant trapped and triggered by complainant’s fast move. The accused failed to show any likelihood at all of a second round of sexual intercourse at the sauna.
[156] Complainant is trustworthy on the facts that after they exchanged kisses and heavy petting, he had protected anal intercourse on the accused and the accused followed doing the same to complainant. That is it and it ended there.
[157] The discrepancies or differences in the testimonies of both regarding saves, their being given or purchased, and even complainants erroneous thought he had two saves, one for him and one for the accused does not at all have any impact on the assessment of the evidence heard. Indeed it demonstrates that sauna for gays are a lieu of gathering for sexual purposes and that practises may vary from one to another and that complainant attended other saunas for gays.
[158] For the Court, there is no doubt whatsoever even through the acknowledged frailties and weaknesses and possibly untrustworthiness of part of complainant’s testimony that it is not at all likely that the accused had before unprotected sex before in saunas for gays. No such admission is recognized as having been made to the accused by complainant. It is not at all believed and was simply invented and meant to serve the accused allegation of implicit consent and unprotected intercourse generally on the part of complainant.
[159] The accused in the opinion of the court would certainly never have admitted any responsibility in his October 14 2006 E-mail if at any time complainant would not have challenged him and said he was forgiving him for that.
[160] The circumstances of the case, the trustworthiness of the complainant on the fact he never engaged before in unprotected sex and the timing of the first symptoms whether compatible or incompatible with the HIV infection do not in the opinion of the Court open any such possibility that the accused was engaged in the past in risky sexual intercourses that could explain this HIV infection confirmed in May or June 2006 after negative testing in September and a few weeks worrying likely symptoms of infection.
[161] The testing of complainant yearly even in 2004 does not necessarily mean the engagement of complainant in significantly risky sexual intercourse. It is simply a tool useful for active gay people in their sexuality and in this case, complainant is believed that this evidence does not justify in the present context question complainant’s HIV status before July 2005.
[162] The alleged admission by complainant that at his initiative he admitted his risky HIV sexuality is totally disbelieved as that is disqualified by the content of the accused E-mails as it is sure that he would never have ventured any expression of sorrow or regret or responsibility. It was on the part of the accused a tricky invention to give hopefully substance to his implicit contextual consent alleged.
[163] Indeed, he did attribute complainant some responsibility of having unprotected anal intercourse saying he had been candid and vulnerable. The accused behaviour and warnings were also a way of saying to complainant he would not have became infected if he had been careful in his dealing with him. Why confess that much if complainant had disclosed a truly significantly risky behaviour? The accused had to believe that there had been no prior unprotected significantly risky sexual behaviour on the part of complainant.
[164] The accused was very firm after disclosure that complainant had to be careful until the results would be known. And that was within those immediate months that followed the residence unprotected intercourse and more than 2 months after the meeting at the sauna. A simple unprotected anal intercourse was considered even when the anus was submitted to the pre-ejaculatory liquids of someone excited, to some risks as these liquids could forthwith be emitted at the time of penetration… even so more when the accused penis had already ejaculated and not been cleaned and evacuated of the post ejaculatory liquids.
[165] As the Court stated, any pretence of prior to the Sauna gathering risky sexual behaviour on the part of the accused is disbelieved and does not hold. Unbelievable that the accused would have admitted to having sex openly and in a significant risky way in saunas or with others in unprotected anal intercourses with others before and after the July 2005 intercourse with other gays That admission is not believed as the accused would certainly have contested his responsibility in his October 14 E-mail and not simply attempted to share the responsibility of the HIV infection with the accused.
[166] The accused is totally disbelieved on his account that he is the one who took the initiative of disclosing his HIV positive status.
[167] That obligation to disclose legally is binding from the time a partner who is HIV positive engages in a significant risky sexual intercourse.
[168] This affirmation that he is the one who at his own initiative disclosed his HIV positive status is disbelieved.
[169] The accused has confirmed by E-mail his inability to disclose his HIV positive status. He describes it as such a « dirty little secret »[32], He clearly does not have the guts and honesty to so disclose. This is exactly the same crucifying and humiliating truth he will not disclose later on to someone he considers so much more important in his life, his February 2006 love or first love ever named D..
[170] The accused conveyed that disclosure on due time was a most difficult and mortifying admission to make. Clearly he is shameful to have to disclose his HIV status as he feels it does not concern the public. It is totally unlikely that the initiative of disclosure originated from the accused. In that E-mail, he undertakes to act responsible and disclose in the future his HIV status. It can only be so because he did not disclose his status to complainant.
[171] How can it be understood in these circumstances that the accused would have flagged that much and disclosed his HIV positive status immediately after his unprotected intercourse at his residence? He did nothing alike at his initiative.
[172] The complainant’s alleged reaction after disclosure is that it is believed he was infuriated and that if it can be believed that the accused spoke of his own difficult experience of getting to know he had become HIV infected, it is totally unlikely that complainant spoke at that period of marriage and offered that much. Exclusive dating was certainly not discussed either at that time. Then dating in that context does not necessarily entail sexual intercourse, does not exclude it but makes it most difficult to believe that both complainant or the accused knowing the accused reaction would have gone further in more significant risky sexual behaviour.
[173] It is reasonable to think that the accused at the time of disclosure described how he got to contract the HIV infection and his reactions to becoming so infected. It is also likely that they had discussions on the HIV infection and careful attitudes to maintain and testing to be done. But the accused in the way he disclosed complainant’s reaction, annihilates any complainant’s allegation of anxiety, fear, anger and that is unlikely.
[174] Whenever there were discussions about the complainant life, history, of being homesick or having lived difficult a difficult relationship with his father, it was not the center of their first discussion and it is believed that these specific discussions were made at some other time.
[175] If there were any marriage discussions, it is likely that it happened at the time of discussions regarding dating and it could only be made at complainant’s initiative as they discussed dating. Exclusivity was clearly not part of the accused intentions and he was blunt with that. He did not reach an intensity of love and appreciation that was to have him engaged.
[176] The evidence does not permit to believe that the accused is the one who took the initiative to disclose although he could have been worried lightly about cross-stains as he did put it.
[177] The perspective of being or becoming HIV has developed in the day of work of the accused and even without there having been the traumatic intercourse referred to, that anal intercourse gave reasons to complainant to be worried as this was not his believed course of action when engaging in sexual intercourse and as it was significantly HIV sexually risky. The court does not doubt that complainant did not have unprotected sex with anyone else than the accused.
[178] The Court finds likely that the accused invited complainant to have only safe sex until the results. That is logic for anyone informed of the risk of being infected. The accused did not speak in an insensitive way but hoped for the best for complainant.
[179] The accused can be believed to have been at best incoherent and if complainant had undertaken not only protected but also unprotected sexual intercourse, he would be incoherent as well. It appeared clear that they had convened that therefore there would be no significantly risky sexual behaviour in between the two. That had truly frightened complainant and it cannot be doubted.
[180] How can it be understood that a careful accused warning complainant would have after July 2005 risked that complainant be submitted to the trauma of a joint penetration of a huge dildo and penis? This pretence is most difficult to believe for both of them.
[181] The first September symptoms that are compatible with an HIV infection do not exclude incompatibility with any other findings. These symptoms gave force to the allegation of an unprotected significantly risky intercourse with the accused in July 2005. Further symptoms showed up in January 2006 and kept on burdening complainant.
[182] That does not exclude in theory the possibility of risky sexual intercourses by both the accused and complainant between July and October 2005.
[183] Complainant has admitted entering at fall a new relationship with a person who has become his companion since then, with whom for a portion of the time he had protected sexual intercourse and never developed an HIV infection.
[184] Most difficult and incoherent for the accused to engage at any time after July 2011 in a dildo penis penetration significantly risky after he would have told the accused to be careful until the tests were done.
[185] More surprising even when the accused states that the dildo was a larger than usual one and that there was at the same time an ensuing joint penis penetration.
[186] There is a strong reason for complainant to be trustworthy as in July 2005 at the accused residence, not only did complainant allege that it was the time of a joint dildo penis traumatic anal penetration as he only became aware at the last moment that there would be an unprotected penetration.
[187] At the time of the joint dildo penis penetration, the accused thought that complainant had not seen him going to engage in an unprotected penis and dildo penetration. That is a very strong argument that will be weighed against the complainant’s testimony from August on.
[188] If in theory and there is no such admission, complainant would have done so in full awareness after July 2005 and risked that much, he could be qualified of being totally incoherent and reckless.
[189] Strangely enough the accused had said that complainant could not see if he was wearing a prophylactic whereas complainant said he became aware of it as it was happening. The accused version is so surprising and close to total unlikelihood, as he would have been reckless and acting contrary to his own recommendations. He would have done so with the impression that complainant was unaware of the fact apart from the dildo penetration, he was about to have a joint penis penetration.
[190] The different account as to the form of the dildo or as to the position of the sexual partners at that very time is noted but does not help the Court to come to a judgment.
[191] The Court cannot exclude the very light possibility of the anal intercourse at the accused residence not being a joint dildo penis traumatic anal intercourse. It could have been an ordinary anal sexual intercourse that ended up worrying the accused.
[192] This very light possibility of an ongoing risky unprotected anal sex intercourses is so close to being frivolous stems from evidence as a whole and more specifically of the frailties of some of complainant’s questionable or even untrustworthy statements.
[193] Complainant offered some understanding that there had been ongoing sex and an intention to keep on dating although he contests strongly having intended to say that much.
[194] Complainant is also confronted by the gatherings acknowledged although in confused or vague ways by him regarding dating or behaving and being presented as a boyfriend by the accused. The trustworthiness of complainant on his denials of unprotected and protected intercourses after July 2005 is under attack even though he might be right.
[195] A slight doubt surges whether the dildo penis penetration happened in or after the month of July 2011. The Court cannot set aside a light possibility that both kept having unprotected sexual intercourses. Even if unprotected intercourses would objectively surprise, in fact, it is not impossible. Coherence in sexuality is not always evident. The magic thinking about the safety of withdrawal before ejaculation in unprotected anal sex might have to do with that.
[196] The accused testimony and the one of his friends combined to the contradictions and frailties of complainant’s testimony, raise a doubt as to when there was that most significant risky sexual behaviour. On that specifically, the Court reads a doubt as to dates and a doubt benefits the accused regarding that aggravating factor.
[197] Dating may not always include sexual intercourses even if there was some overt expression of affection, of tenderness, of love. It surprises as the accused does not have much of a favourable opinion of complainant and dislikes him sexually. That would tend to undermine any pretences of a love relationship in the public eye of his close friends. But there was dating and a love feeling is not essential for all to become involved sexually.
[198] Also the rental of his residence to complainant may question the accused motivation in dating complainant, his wanting to buy peace and consolidate conditions to avoid any criminal pursuits. It does not mean per se that all of that is illegitimate. It does not set aside the doubt born out of complainant’s frail testimony on his after July gatherings and communications with the accused.
[199] Whatever united the accused and complainant was love as difficult as it could be, as hopeful as it could be, as limited in perspective as it could be, as injured as it could be because of that possibility if not likelihood of complainant being infected by the accused. But, these were two intelligent persons who dealt intimately with one another.
[200] But complainant gave overt reasons to believe that there could be an ongoing intimate relationship, ongoing discussions, ongoing dating, ongoing expression of gestures of sensuality and love after July 2005.
[201] That questions complainant’s coherence as alleged by the accused. Complainant has a credibility gap as to what happened with the accused after July 2005. Complainant’s falling in love with his present partner at the beginning of fall 2005 does not exclude an interim period where both complainant and the accused continued to date one another and still getting involved in more intimate intercourses.
[202] But it is the opinion of the Court that on the whole of the evidence, the lack of trustworthiness of complainant does not affect at all the accused allegation of no unprotected evidence with others at all relevant times before the sauna incidents and after the sauna incidents save for his relationship to the accused.
[203] These doubts do not question complainant’s trustworthy account of the sauna and residence intercourses and non-disclosure and how there was disclosure. These doubts do not extend to complainant’s sexual behaviour with others before and after July 2005. The accused exposed complainant to a significantly risky HIV infection.
[204] These doubts are raising the question of complainant engaging in sexual partnership and sexual intercourses with the accused from August on. Complainant’s trustworthiness lacks specifically there and not on his absence of unprotected sexual intercourse with others and not on his unwillingness to engage sexually with someone HIV infected in July 2005.
[205] Clearly complainant would have never engaged in unprotected significantly risky sexual intercourse with the accused if there had been proper disclosure. There and then the elements of the commission of the infraction were established.
[206] The accused testimony was found to be vague, general, at times relying on their constant sexual practises and even argumentative as to their ongoing unprotected and unprotected intercourses. But complainant’s untrustworthiness on dating and ongoing sex and his very vague testimony some of it that would be understandable alike the one of the accused, does raise a slight doubt on the date of that fatal significant risky joint dildo penis intercourse.
[207] The Court is also puzzled by the testimony of complainant. It is not likely that he kept in touch with the accused solely to keep track of him. They kept on dating and it is confirmed that there was such apparent dating.
[208] Complainant who stated that he got aware at the very last moment that the accused would do on him a dildo penis unprotected penetration is confirmed as to that specific intercourse by the accused who doubts that complainant could see what he was doing. Both have a different description of the position of the accused at the time of that intercourse and of the dildo used and of dildo gifts thereafter. The court does not know who says the truth on positions. It is difficult to believe that the most significant risky HIV joint dildo penis penetration did not happen in July. But that slight possibility cannot be excluded as balance of probabilities is not the test and as complainant’s testimony regarding events after July 2005 has been at times questioned and confused and untrustworthy.
[209] Complainant strangely referred to having friends of whom he did not know the HIV status, as he was not even put the question of him engaging in any sexual intercourses with them for the period of July 2005 to October 2005. He also denies any sexual intercourse with anyone else and he is believed.
[210] Throughout he always said he had no unprotected intercourse with anyone save the July one with the accused and further that he had none after July with the accused. On that a doubt remains because of his declaration as to ongoing sex and wanting to keep dating and because of the frailties and contradicted evidence of complainant in the months of August and October 2005.
[211] It has to be remembered that it was the accused who allegedly wanted not to enter an exclusive sexual relationship with complainant as he had at that time a lover.
[212] Complainant’s behaviour is believed to show ongoing dating. In the course of this lack of credibility of complainant as to dating, a doubt surges regarding ongoing sex practises.
[213] Ongoing sexual intercourses with the accused until October is a possibility that cannot be ruled out. Complainant said so in a question to the accused in his recorded 2006 interrogator as he says in a preamble that they kept having sex and that they wanted to keep on dating.
[214] That is a flaw in complainant’s version that leaves the Court abashed and unable to conclude that the joint dildo penis incident that could indispose complainant could not have happened after July although the accused testimony is close to being on major aspects of the July incidents untrustworthy and questionable. It is not that the accused did not admit to that significant sexual intercourse at least at his residence.
[215] The Court can certainly not infer from the accused being untrustworthy on most aspects his guilt as complainant has himself through his behaviour, and version raised a doubt on the date of the joint dildo penis penetration that was and is fatal on his becoming HIV infected. This is where prosecution fails its burden of establishing the aggravating factor of the accused infecting complainant.
[216] The burden on Prosecution is not a burden of establishing on a balance of probabilities or alike in some other countries that it suffices that the judge has developed a moral conviction of the accused guilt. That is not the test. And it is essential for a justice system and for a perception of justice rendered that the burden of evidence be as it is here, namely that the accused guilt be established beyond a reasonable doubt.
[217] It goes per se that no scientific tests could help decide if the infection was caused by the accused in July or thereafter.
[218] The Court cannot come to a definite conclusion that the fatal unprotected intercourse dated to July or thereafter although there is a very strong possibility with the symptoms that it was caused in July before disclosure.
[219] That questions and raises a doubt as to the denial of complainant on the continuation of the sexual intercourses. Complainant’s denial was radical. It is being questioned by circumstances and a possible truthful allegation of the accused that they did continue to have both protected and unprotected sex. This makes it difficult to believe beyond a reasonable doubt that the first sexual intercourse at the accused residence happened as stated by complainant by a dildo penis penetration or that their sexual encounters ended there. But there is no doubt that there was an anal penetration that per se is a significant risky HIV sexual intercourse even if exposed solely to pre-ejaculatory liquids of the accused.
[220] If that traumatic intercourse would have happened at the residence of the accused and would have indeed scared complainant as he says, it is doubtful that complainant would have continued dating or having unprotected sex or would have kept that way in touch with the accused simply to keep track of him.
[221] Indeed the reasonable possibility cannot be set aside that they kept on having that protected and unprotected sex and that the May and June 2006 testing was passed so late as a consequence of a later than July traumatic sexual intercourse with the accused. It could go both ways time wise. But there is evidence that cannot set aside as complainant has been contradictory and untrustworthy and vague and confused on some of the evidence after July 2005 to August 2005.
[222] That traumatic intercourse could certainly be a source of greater concern for complainant and could also contribute to explain why anyone would delay further a test that could have been passed a few months after the time recommended. Complainant would not have felt as vulnerable after the July intercourse if it was a straightforward unprotected anal intercourse risky but never as much as the one with the dildo and penis penetration. The first negative test of September 2005 could also have tricked both in indulging in more.
[223] After the last June 2006 tests, the October 2006 invitation to the accused to confess with the promise he would be forgiven, trapped him into admitting his responsibility, saying how sorry he was. At the same time, the accused attempted to share the responsibility of whatever went on between the parties.
[224] If there were sexual intercourses after July 2005, complainant is the one who took the ultimate risk and responsibility of been carried in risky sexual behaviour and of being contaminated by the accused HIV infection if it had not already contaminated him.
[225] The Court does not believe in jealousy being key to the criminal pursuits by complainant. Seeking justice certainly prompted the accused to lay a complaint. Complainant appeared a man much hurt and the accused has the right to a verdict that gives way to whatever reasonable doubt flows from all of the evidence heard.
[226] The care complainant took to pass HIV tests every year and the absence of significantly risky sexual behaviour prior to the meeting the accused leaves no doubt that the accused did put at risk the life of complainant in July 2005 as was not disclosed by the accused his HIV positive status.
[227] The state of health of complainant in September is worrying and would permit to anticipate the first symptoms of the HIV infection. But the Court would have readily concluded to the HIV infection of complainant in July 2005 if there had been no doubt whatsoever that the traumatic most significantly risky happened in July 2005 and that these symptoms were associated without any doubt in time to July intercourse.
APPLICATION OF LAW TO THE FACTS
[228] This case offers a straightforward application of the Cuerrier stay of the Supreme Court of Canada.
[229] Prosecution had to establish beyond a reasonable doubt that the accused’s acts endangered the life of complainant as there was no disclosure, no implicit consent and as complainant would never have accepted to have sexual intercourse with the accused if he had been informed and the significantly unprotected sexual intercourse at the accused residence (section 268 (1) and 272 of the Criminal Code).
[230] Complainant was not infected before meeting the accused. There is evidence to so believe beyond a reasonable doubt that complainant was not then infected. Complainant and the accused engaged in an unprotected sexual intercourse at the accused residence that was significantly risky according to the ruling of Cuerrier. The guilt of the accused is established by the simple exposure of complainant to a significant risk of HIV infection before any disclosure was made, as complainant would never have entered a sexual intercourse with the accused if there had been disclosure by the accused of his HIV infection.
[231] The expert Dr Morrissette stated very clearly that the HIV infection is lethal and endangering life when complainant was sexually assaulted.
[232] The anal unprotected intercourse represented a significant risk just through complainant’s anal exposure to the pre-ejaculatory liquids of the accused.
[233] The Court makes the finding that the accused intentionally applied force against the consent of the complainant. Fraud, dishonesty of the accused sufficed to vitiate consent. That had to be assessed objectively to determine it. This was so as consent was not to simply engage in sexual intercourse but to have sexual intercourse with a partner who was not HIV positive. That dishonesty of the accused had to be such as exposing the complainant to a significant risk of serious bodily harm, as HIV has been so characterised.
[234] As dishonesty has to result in deprivation, both the risk of the HIV infection, AIDS as well as that actual harm meet the test by establishing that that dishonest act had such an effect of exposing complainant to that significant risk of bodily harm.
[235] In this case, the accused who to his knowledge was HIV positive since 2003, did not disclose his HIV positive status at any time before the sexual July 2005 gatherings were through. He knew that he could not irresponsibly put the life of anyone at risk in abstaining disclosing is HIV positive status with significant risky sexual activities.
[236] There was no consent whatsoever by complainant to be exposed to such a risk. Consent had to be clear and unequivocal and such was not the case. There was no contextual implicit consent of complainant that could be inferred subjectively from the whole circumstance. The accused was truly dishonest and exposed complainant to a risk of harm that was not trivial but of serious bodily harm that is fatal, lethal. The accused knew it and admitted he was unable to disclose that dirty little secret.
[237] There was only disclosure once confronted by complainant after an unprotected anal penetration.
[238] The Crown had to show that complainant would have refused to engage in unprotected sex with the accused if he had been advised that the accused was HIV positive. The evidence is to the effect that complainant would not at all have accepted to have any sexual intercourse with the accused if he had been advised. Complainant is believed and trustworthy.
[239] The aggravating factor of the HIV infection of complainant prior to August 2005 is not established beyond a reasonable doubt. In criminal matters, there is one and only one test and probability even to a very high degree is not sufficient for a verdict of guilt. Evidence of guilt has to be established beyond a reasonable doubt. The likelihood of complainant’s version does not suffice on the aggravating factor. Complainant’s version of the evidence regarding the timing of the incident of the dildo penis traumatic sexual anal intercourse is shaken but not defeated or shaken anyway as to its happening. Complainant’s version has been shaken as to the continuation of the sexual partnership after disclosure.
[240] It makes a huge difference that this undoubtful causation of complainant’s HIV infection may have happened only probably in July 2005 before disclosure and nonetheless possibly after disclosure. The trustworthiness of complainant’s version as to most of what happened before disclosure did establish beyond a reasonable doubt the guilt of the accused on the infractions as laid.
[241] The accused did his best to be so nice with complainant so as to deter complainant to lay a complaint to the police and avoid criminal pursuits.
[242] As the Prosecution has demonstrated beyond a reasonable doubt the guilt of the accused by exposing complainant to the HIV infection in engaging with him on one occasion before disclosure in an anal unprotected intercourse, the accused is guilty of the infractions, as the accused has been indicted with. There was an assault at the residence of the accused irrespective of complainant being infected and the accused was not at all HIV positive before the July 2005 sexual assault.
[243] The accused is guilty of either of these infractions. But there will be a stay of proceedings on the count of aggravated assault as this infraction situates rightly the wrongful and illegal behaviour of the accused and this is precisely the whole behaviour of the accused that is denounced.
THEREFORE THE COURT DECLARES THE ACCUSED GUILTY OF THE INFRACTION OF AGGRAVATED SEXUAL ASSAULT ENDANGERING THE LIFE OF PWD.
THE COURT STAYS THE PROCEEDINGS ON THE COUNT OF AGGRAVATED ASSAULT IN APPLICATION OF THE KINEAPPLE STAY.
__________________________________
LOUIS A. LEGAULT, J.C.Q.
Me Sarah Henningson, Me Sophie Lamarre
ATTORNEY FOR THE CROWN
Me Jeffrey Boro
ATTORNEY FOR DEFENCE
Dates of hearing:
10 December 2009, 28 April, 25 June, 20 and 21 October, 16 December 2010, 29 August 2011


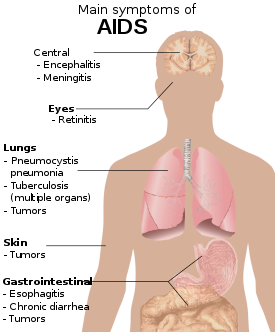



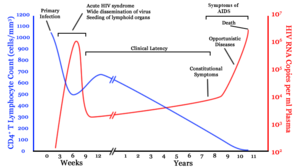







 Organized by African Men for Sexual Health and Rights (AMSHeR), the meeting dubbed ‘Claim, Scale-up, and Sustain’ seeks to increase attention on MSM and HIV related issues in Africa, to reflect on the state of the response in MSM communities in Africa and to identify ways forward for scaling up MSM and HIV interventions, according to News from Africa website.
Organized by African Men for Sexual Health and Rights (AMSHeR), the meeting dubbed ‘Claim, Scale-up, and Sustain’ seeks to increase attention on MSM and HIV related issues in Africa, to reflect on the state of the response in MSM communities in Africa and to identify ways forward for scaling up MSM and HIV interventions, according to News from Africa website. The idea of the ‘Tombstone ad’ was to shake a nation into taking charge of its own sexual health
The idea of the ‘Tombstone ad’ was to shake a nation into taking charge of its own sexual health

 The message correlates masculinity and responsible sexual behaviour
The message correlates masculinity and responsible sexual behaviour A 2005 billboard campaign against HIV/Aids outside a university in the Niger Delta
A 2005 billboard campaign against HIV/Aids outside a university in the Niger Delta Sting: King met an undercover police officer at Waterloo Station, who he thought was going to allow him to abuse children
Sting: King met an undercover police officer at Waterloo Station, who he thought was going to allow him to abuse children
